The COVID-19 pandemic has highlighted—and exacerbated—the gaps in healthcare systems in lower- and middle-income countries (LMICs). Prior to the pandemic, almost a third of the population in those countries lived more than two hours away from essential healthcare services, and the ratio of healthcare workers to population was typically well below the minimum recommended by WHO.1 The loss of healthcare workers to COVID-19 and the disruption of transport systems because of lockdowns have worsened the impact of these issues.
However, a silver lining of the pandemic has been the growth in digital tools, with companies reporting an acceleration in the adoption of digital technology by several years. Digital technologies have tremendous potential not only to improve countries’ responses to infectious-disease threats but also to strengthen primary healthcare. McKinsey and the Exemplars in Global Health have had a yearlong research collaboration focused on assessing digital tools for primary healthcare in LMICs (prioritizing those used during the COVID-19 pandemic) to understand how to harness digital tools to transform primary healthcare systems and to achieve step-change improvements in healthcare.
Achieving such improvement will not be easy, however. To realize the promise of digital healthcare at scale, strong country-led partnerships and enabling environments will likely be required in most instances—and the effort will likely need to focus on known, adaptable technologies and user-centered design. Along those critical success factors, LMICs will likely be expected to focus on effective capability building, sustainable business models, and rigorous monitoring and evaluation.
If LMICs apply these success factors, they could strengthen and broaden the use of digital tools across multiple use cases in primary healthcare. LMIC governments and their partners could then continue toward their goals of shaping the national healthcare ecosystems that connect multiple healthcare journeys and aggregating data for seamless user experiences.
The analysis presented in this article delves into the success factors that can drive effective, widescale implementation of digital tools across healthcare systems in LMICs. Following a four-part methodology, our evaluation draws on analysis and interviews with leaders in governments and international organizations and with expert digital-solution developers. We then offer a vision of the digital-healthcare landscape for primary healthcare in LMICs and propose potential pathways to drive the implementation of digital healthcare to realize that vision.
Successful implementation of digital tools: Lessons for LMICs
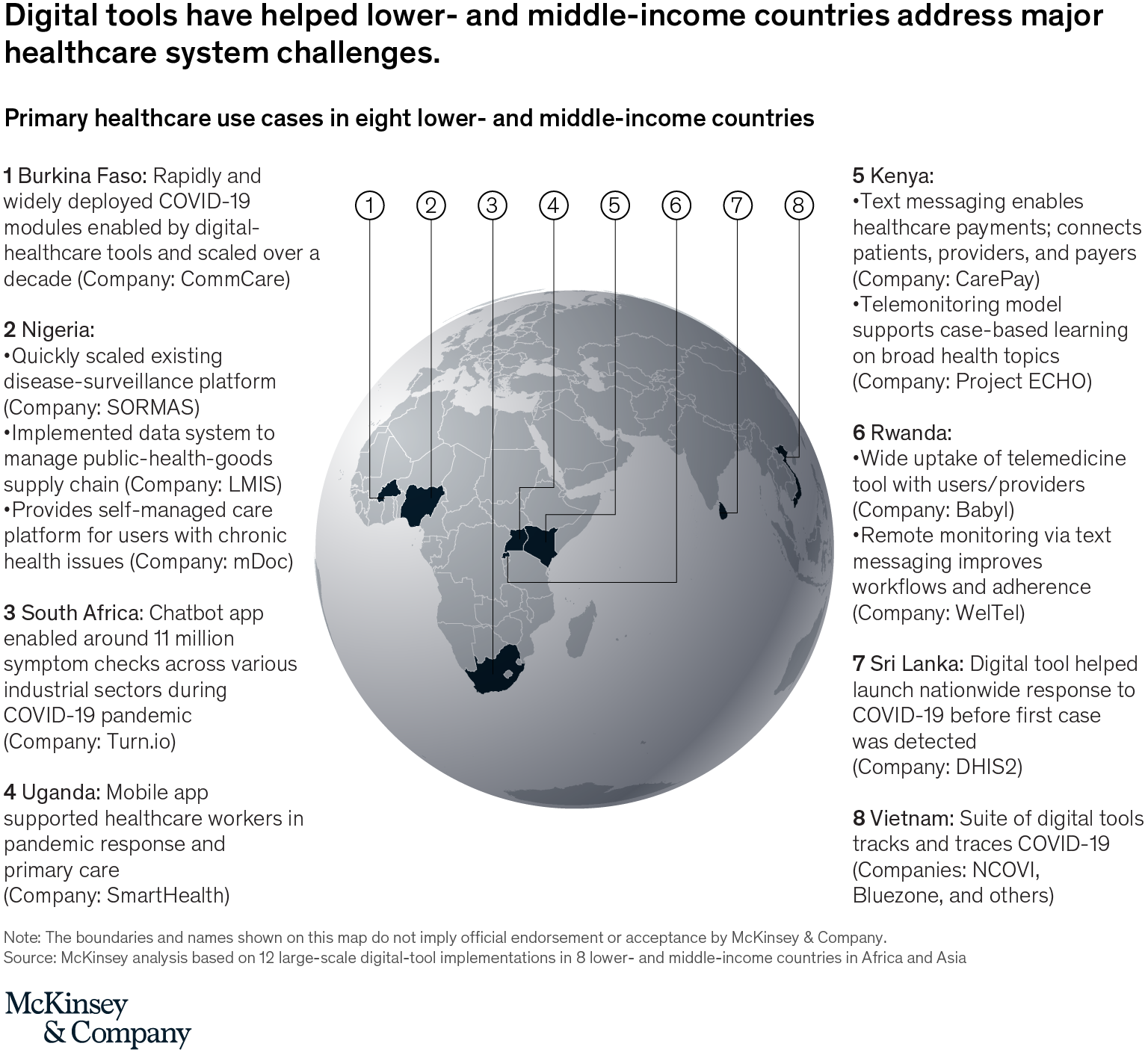
The knowledge collaboration that forms the basis of this article assessed 12 large-scale digital-tool implementations (Exhibit 1), highlighting use cases for primary healthcare in eight LMICs in Africa and Asia (see sidebar “Methodology: Prioritizing tools for digital healthcare”). Through the analysis, we identified six success factors that have contributed to the ability of digital solutions to scale and achieve impact: strong, country-led partnerships; known and adaptable technologies; user-centered design; sustainable business models; capability building; and monitoring and evaluation.
The first three factors are the most critical for quickly implementing a tool at scale, and most of the successful digital solutions in this study consistently applied them—which also helped patients during the COVID-19 pandemic. The last three factors also contributed to the achievements of some of the tools assessed and are important to ensure longer-term success.
Strong partnerships among governments and digital-solution providers can drive scale
Digital-solution providers and governments often have interlocking relationships when deploying large-scale solutions. In settings in which governments and nongovernmental organizations are ill equipped to build and deploy solutions on their own, technology innovators have a critical role to play. Solution providers can evaluate how to integrate with government systems and may depend on strong, top-level government leaders to champion system change and drive user adoption.
It is important to establish relationships and credibility with other trusted and already-established stakeholders at an early stage.2 Partnering with established organizations, service providers, or government agencies is often vital to reaching scale. In Kenya, for example, foundational in-country partnerships established prior to the COVID-19 pandemic leveraged the partners’ deep market understanding and consumer experience. To date, M-TIBA, a financial-technology platform, has connected more than four million users and 1,200 healthcare providers in Kenya.
Working with governments to foster longer-term partnerships helped many developers achieve scale and act quickly in response to the COVID-19 pandemic in several countries. In Nigeria, for example, SORMAS, an open-source, mobile e-health platform, is a product of a yearslong collaboration between the Nigeria Centre for Disease Control and the Helmholtz Centre for Infection Research in Germany. The partners drew on the country’s experiences with Ebola and monkeypox, allowing the program to grow from its initial concept as a process-management tool to a full health-surveillance platform. This meant it was well positioned for a large-scale, complex outbreak, such as the COVID-19 pandemic. SORMAS expanded deployment in Nigeria from 15 states covering 75 million inhabitants in 2019 to 36 states covering all 206 million inhabitants in the country in 2020.3
Other examples of partnerships among governments and digital-solution providers include Turn.io’s chatbot app, which allowed more than 11 million symptom checks in South Africa, and the Vietnam Ministry of Health’s launch of a suite of digital tools, including NCOVI and Bluezone, to respond to the pandemic. As of March 2021, Bluezone had been downloaded by 24.2 percent of the population, and NCOVI had been downloaded by 19.8 percent of the population, allowing users to receive critical health information during infection spikes.
Adaptable technologies allow rapid customization
To achieve scale and impact, it is essential to develop a stable, reliable product that can improve and adapt over time. Rather than developing brand-new solutions, many programs in our study used existing technologies, which, in some cases, were digital public goods.4 For example, Praekelt was able to build on existing ongoing work with the South African National Department of Health to support maternal health with MomConnect, which uses mobile-phone-based technologies. This enabled it to develop the COVID-19 Connect South Africa platform and roll it out within weeks. Seven weeks after launch, more than 6.2 million users had joined the platform, with approximately 750,000 using it daily. While that was only a fraction of the country’s 59 million inhabitants, the uptake during the COVID-19 pandemic has been notable.
In another example, Living Goods, using a Medic-designed mobile-health solution, was able to adapt its service-delivery model rapidly with new workflows related to the COVID-19 pandemic and increase treatments by more than 30 percent in all categories, doubling the estimated number of lives saved compared with the previous year.5 A major success factor, in addition to established partnerships and effective collaboration, was the authority of local teams to make decisions, which reduced product-development timelines to two weeks, from multiple months. Based on interviews, CommCare also had a clear troubleshooting hierarchy in place in Burkina Faso, with regional repair teams deployed to escalate and address users’ technical issues quickly. With rapid adaptability, such as Medic’s, this operating model was instrumental in adapting to the pandemic.6
In addition, working with interoperable models or ecosystems supported by agile teams can make it easier to adapt solutions to meet local requirements. For example, Nigeria Health Logistics Medical Information System is interoperable with warehouses and its electronic proof-of-delivery system, allowing it to provide detailed inventory levels and proof-of-delivery data.
User-centered design enables the establishment of a clear value proposition
The foundation of a successful digital tool is in defining the value of the solution—both the problem it seeks to address and for whom it is intended—up front. Developers may seek to design a human-centered solution that is aligned to user priorities and market research and is supported by an initial proof of concept. A necessary consideration is whether there is an enabling environment for the envisaged solution (such as whether the proposed design is appropriate for the digital skills and connectivity of the target market).
When the not for profit Living Goods partnered with Medic to design the SmartHealth app, for example, Medic developers spent several weeks in communities in Uganda to understand the workflows related to healthcare workers connecting with patients. Their study included potential pain points, communication channels, and the infrastructure that may be required to support a digital platform. In Kenya, Living Goods started with a fully self-financed pilot to demonstrate proof of concept and earn credibility. CarePay collaborated with different stakeholders—healthcare providers, commercial partners, and funding partners—in the development of its app to provide an integrated platform for payers and savings for clients.
Sustainable business models contribute to long-term financial viability
Related to a clear value proposition, the development of a business model that demonstrates value to user groups can help a digital solution go beyond donor investment and ensure its sustainability. While this has been a pain point for many digital solutions, and all have some way to go, a few have offered promise in this regard.
In Nigeria, for example, mDoc is working to develop two revenue streams. Its platform connects users with a care team and with monitoring tools for self-management of chronic diseases, with one revenue stream based on a B2B model involving service fees paid by health-maintenance organizations and employers and a second on a B2C model with monthly subscriptions. In Rwanda, Babylon (Babyl) has adopted multiple revenue streams, including subscription-based and pay-as-you-go services, as well as centralized funding, such as the government’s community-based health-insurance program.
Successful solutions can also realize predictable value by digitizing and standardizing processes. For example, Medic and Living Goods are automating and standardizing task and decision-support lists for community healthcare workers, shifting their workflows from reactive to proactive or predictive outreach, which could save costs over time.7
Capability building supports effective operations
The capacity to use tools and change management are key enablers of helping scale digital solutions. For example, Dimagi worked with Terre des hommes and the Ministry of Health in Burkina Faso to transfer knowledge on the CommCare platform so that organizations could manage the solution independently.
Building in change management up front is crucial for scaling, and we also see it as critical for securing longer-term, enduring solutions. The implementation of Nigeria Health Logistics Medical Information System required change management across all levels of stakeholders—from leaders to technicians—to ensure adoption at scale over time.8
Monitoring and evaluation enables adaptation to evolving needs
Rapid evaluation and reformulating of services to suit local contexts and requirements in line with government priorities allows developers to build long-term relationships and trust with users and governments. In addition to sustainable business models, strong monitoring and evaluation processes were lacking across many of the digital-solution implementations we studied. Rigorous and outcome-driven evaluation is important with the implementation of any new or existing tool.
For example, WelTel ran several trials to understand how, when, and why its platform was effective. That knowledge not only helped the company improve its platform in Rwanda but also led to the solution’s implementation in high-income locations such as Vancouver, in Canada, and Seattle, in the United States.9
A national digital-healthcare ecosystem for the greatest impact
In our analysis of digital solutions and their use cases, we also looked at how they might relate to and connect with one another in the context of the broader healthcare system. This assessment was done along the parameters of potential scale and level of integration of different user journeys (see sidebar “Methodology: Defining potential end states for digital healthcare”).
The current digital-primary-healthcare landscapes of most LMICs are characterized by fragmented solutions, with some examples of national-level excellence along a single healthcare journey. Depending on their current state, LMICs could aspire toward one of three end states in digital primary healthcare10:
- interoperability among multiple healthcare journeys at national level
- a national healthcare ecosystem that connects all healthcare journeys and patient data
- regional interoperability and integration on key use cases, such as cross-border public-health surveillance
While all three end states would contribute to improved quality and user experience, building a national healthcare ecosystem would have the greatest impact. LMICs with the capability could then support regional interoperability on use cases that could benefit from cross-country coordination, such as disease surveillance and contact tracing.
Prioritizing a national healthcare ecosystem can enable data flow and foster collaboration among key stakeholders to achieve the following improvements:
- Expansion of healthcare coverage. Expansion could allow broader reach of healthcare delivery through technological solutions.
- Enhanced quality of services. Better-quality services could support improved coordination of care through data sharing and provide a convenient and seamless user experience. They could also enhance the quality of professionals, providing data and analytics for evidence-based guidelines.
- Resource optimization. Optimization could enable earlier detection of risks through predictive analytics and enable long-term cost management. In the near term, it could also have a significant impact on management efficiency by allowing increased division of labor and overall utilization through centralized, coordinated, real-time management.
Country archetypes to determine implementation pathways
LMICs can consider an enabling environment across six dimensions to advance their digital-healthcare programs toward a national healthcare ecosystem. They can follow a three-step process to identify and start the journey along the optimal implementation pathway for their context. First, they can assess their current baseline state against those six enablers to determine what is needed (Exhibit 2). Second, they can align on the key strategic choices that are available to them (Exhibit 3). Finally, they can define and execute an implementation pathway based on their baseline findings and strategic direction. While all LMICs can aim to build a national ecosystem in the long term, the priority areas for implementation may vary, depending on their current state.


When assessing the baseline, we found that a country’s governance and digital readiness were the key differentiating enablers that defined it as one of the following three archetypes, based on our research (see sidebar “Methodology: Defining implementation archetypes for digital healthcare”):
- a government-led digital-healthcare effort with strong digital foundations (for example, Burkina Faso and Rwanda)
- a private-sector-led digital-healthcare effort with strong digital foundations (for example, India, Kenya, Nigeria, and South Africa)
- a public- or private-sector-led digital-healthcare effort with nascent digital readiness (for example, Angola, Chad, Ethiopia, and Mali)
A country can make strategic choices along the six enablers to guide implementation. Some strategic choices are directly linked to—or limited by—a country’s governance and digital readiness, while others could be explored by all three of the options.
Importantly, however, our research indicates that countries do not necessarily need to follow a linear pathway to achieve a national ecosystem. With concerted government effort and resource support, it is possible to accelerate digital transformation and leapfrog steps in the implementation pathways. In addition, privacy is an essential consideration in the implementation of a digital-healthcare ecosystem, regardless of a country’s archetype or the implementation pathway it follows.
Government-led digital-healthcare effort with strong digital foundations
Countries with a government-led digital-healthcare effort and strong digital foundations could prioritize strengthening the national digital-healthcare strategy by prioritizing data exchange and interoperability at the national level. Governments can intervene directly by creating dedicated teams responsible and accountable for the efforts around digital-healthcare strategy. Countries can also develop mechanisms for sustainable financing of the digital system beyond donor funding.
For example, Rwanda is becoming a digital-healthcare success story, driven by strong country action and strategic partnerships.11 The government has created an enabling environment through its national growth strategy, its 90 percent universal healthcare coverage, and improvement of the country’s digital readiness.12 That includes reliable IT infrastructure, with broadband coverage of more than 90 percent of the population, and focused digital capability building for healthcare workers. Rwanda’s effort to develop the digital-healthcare environment has been strengthened through partnerships, such as the government’s partnerships with Babyl to scale telehealthcare and with Zipline for drone delivery of essential medical products (Exhibit 4).

Private-sector-led digital-healthcare effort with strong digital foundations
Countries with a private-sector-led digital-healthcare effort and strong digital foundations could prioritize data exchange and interoperability at a national level through strategic partnerships with the private sector. That could include developing national digital-healthcare governance with effective mechanisms for collaboration and coordination among public- and private-sector stakeholders. Governments in these countries may also consider digital-healthcare legislation and policies to attract private-sector investment and improve business-case bankability. For example, India benefits from a flourishing digital- healthcare private sector and strong country action to develop a national healthcare ecosystem. The country has a thriving start-up landscape in digital healthcare—for example, healthcare-technology start-ups in India raised a total of $504 million between 2014 and 2018—strengthened by government investment in digital infrastructure that enables digital interoperability.13
Public- or private-sector-led digital-healthcare effort with nascent digital readiness
Countries with nascent digital readiness have the scope to leapfrog steps in the implementation pathway for digital healthcare. The highest priority for these countries is to improve digital readiness by investing in infrastructure and capability building, but they can also build a forward-looking, national strategy that demonstrates the government’s commitment to promoting digital healthcare. With government incentives, solution providers can also start developing critical use cases—such as digital payments to bypass broken financing mechanisms and electronic health records—to prove the concept and lay the foundation for a data-exchange platform.
One example is Ethiopia, which has accelerated its digital journey thanks to decisive action and to cocreation and cofunding partnerships with donors. The country prioritized its digital-healthcare strategy, adopted best practices in data and IT, and fostered a culture of data use at all levels of the healthcare system. It also invested in end-user training and created the Digital Health Innovation and Learning Center to foster innovation.14
Adopting a systematic approach to realizing the vision of a national healthcare ecosystem can improve the application of digital-healthcare tools across LMICs, leading to individual and collective healthcare gains. Stakeholders could prioritize application of the success factors identified in this article to leapfrog digital journeys in LMICs and help a wide range of people lead healthier lives.
This article is based on research collaboration between Exemplars in Global Health and McKinsey. It forms part of a comprehensive set of documents, including a case library, for dissemination and discussion among stakeholders.




